Navigating Blood Sugar: How to Control Diabetes During the Menstrual Cycle
For women managing diabetes, the menstrual cycle can introduce a complex layer of challenges. Fluctuating hormones can significantly impact blood sugar levels, making consistent control a difficult task. Understanding the interplay between menstruation and diabetes is crucial. This knowledge empowers women to proactively manage their health. This article will provide actionable strategies. These strategies help navigate the hormonal shifts and maintain stable blood sugar. The ultimate goal is to improve overall well-being.
The Hormonal Rollercoaster: Understanding the Impact
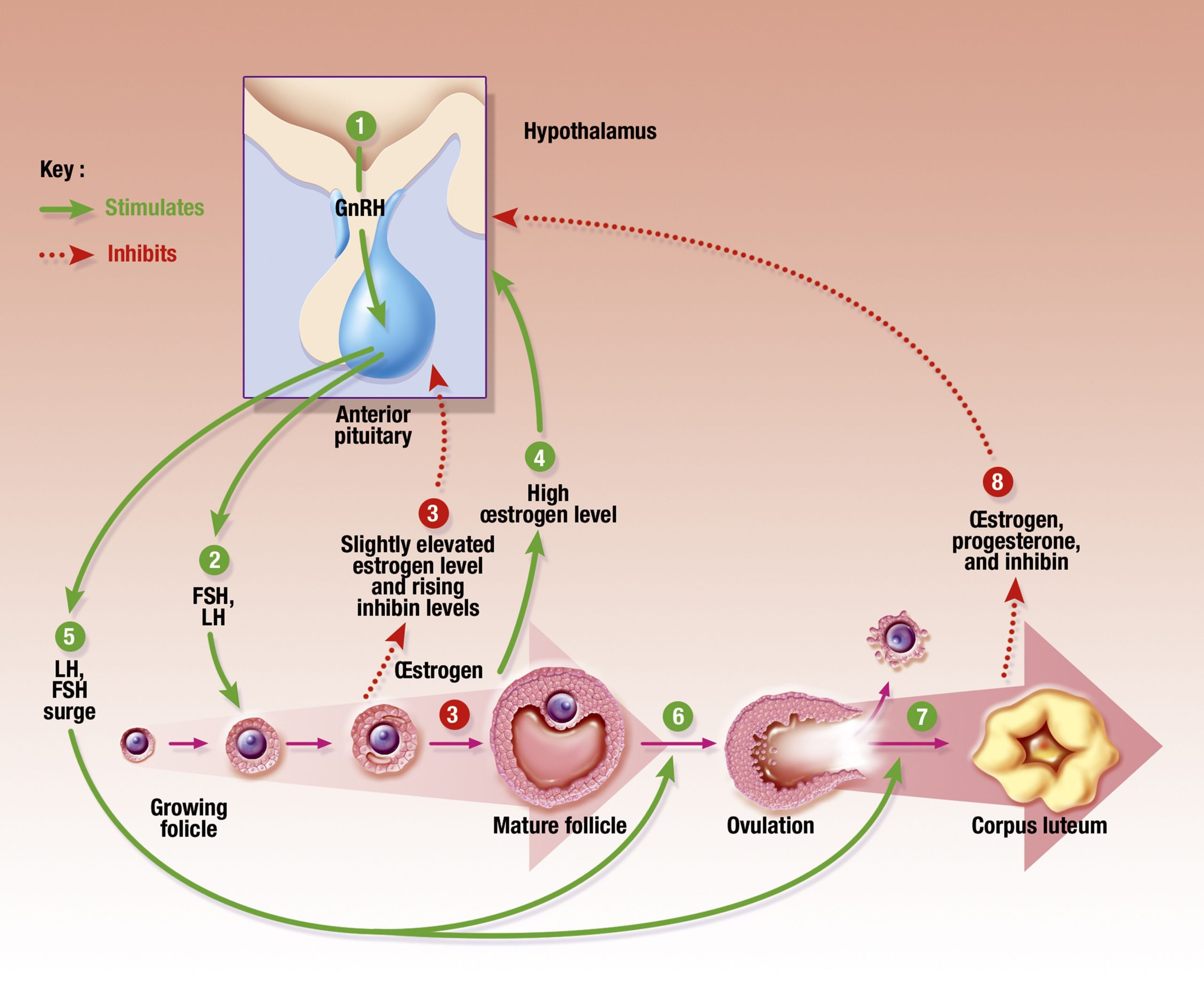
The menstrual cycle is a dynamic process. It involves a complex interplay of hormones. These hormones include estrogen and progesterone. These hormones rise and fall throughout the cycle. These fluctuations directly affect insulin sensitivity. Insulin sensitivity is the body’s ability to use insulin effectively. During certain phases, insulin sensitivity decreases. This can lead to higher blood sugar levels. Conversely, in other phases, insulin sensitivity may increase. This can lead to a higher risk of hypoglycemia (low blood sugar).
Estrogen plays a significant role in glucose metabolism. It influences insulin sensitivity. Progesterone also impacts insulin resistance. Both hormones work together. They create the cyclical changes women experience. The body’s response to insulin varies throughout the month. This variance makes diabetes management more challenging. Women with diabetes need to be extra vigilant. They need to adapt their management strategies.
Tracking and Monitoring: The Foundation of Control
Effective diabetes management during the menstrual cycle begins with diligent tracking. Keeping a detailed record of blood sugar levels is essential. Women should monitor their blood sugar several times a day. They should do this throughout the entire cycle. This data provides valuable insights. It helps identify patterns and trends. It also helps understand how blood sugar levels change over time. A good log should include the date, time, and blood sugar readings.
In addition to blood sugar levels, women should also track other relevant information. This includes menstrual cycle dates, symptoms, and dietary intake. They should also track physical activity levels and any medications taken. This comprehensive approach provides a complete picture. It allows for a more personalized management plan. The more data collected, the better the understanding of individual patterns. This improved understanding leads to better control.
Dietary Adjustments: Fueling the Body Right
Diet plays a critical role in managing blood sugar. This is especially true during the menstrual cycle. Women should focus on a balanced diet. This diet should consist of complex carbohydrates, lean protein, and healthy fats. These foods help regulate blood sugar levels. They also provide sustained energy. Women should avoid highly processed foods. These foods can cause rapid spikes in blood sugar. They should also limit sugary drinks and snacks. These additions can lead to blood sugar instability. [See also: Healthy Meal Planning for Diabetics]
Adjusting the diet based on the menstrual cycle can be beneficial. During the premenstrual phase, cravings for sugary foods are common. Women should prepare healthy snacks. They should have these snacks readily available. These snacks could include fruits, vegetables, and nuts. These options provide satisfying alternatives to unhealthy choices. It’s also important to maintain consistent meal timings. Regular meals and snacks help prevent blood sugar fluctuations. This helps keep blood sugar levels stable.
Exercise and Physical Activity: Moving Towards Balance
Regular physical activity is a cornerstone of diabetes management. Exercise helps improve insulin sensitivity. It also helps regulate blood sugar levels. During the menstrual cycle, exercise can be particularly beneficial. It can help counteract the effects of hormonal changes. Women should aim for at least 150 minutes of moderate-intensity exercise. This should be done throughout the week. This can include brisk walking, swimming, or cycling. [See also: Exercise and Diabetes: A Comprehensive Guide]
It is important to listen to the body. Some women experience increased fatigue or discomfort during their period. During these times, modifying the intensity of exercise may be necessary. Lower-intensity activities like yoga or stretching can be helpful. They can help maintain physical activity. They can also help reduce stress. Women should also be mindful of hydration. They should drink plenty of water before, during, and after exercise. This helps prevent dehydration. Dehydration can affect blood sugar levels. Understanding the impact of exercise on blood sugar is crucial. This understanding empowers women to make informed decisions.
Medication Management: Fine-Tuning the Dosage
Medication adjustments are often necessary to effectively manage diabetes during the menstrual cycle. Women should work closely with their healthcare provider. They should discuss any changes in blood sugar patterns. These discussions allow for informed decisions. These decisions are about medication dosages. The healthcare provider may recommend adjusting insulin doses. They may also adjust oral diabetes medications. These adjustments are based on blood sugar readings and cycle patterns.
It’s crucial to avoid self-adjusting medications. This can be dangerous. Any changes should be made under medical supervision. Regular check-ups with a healthcare provider are essential. These check-ups help monitor overall health. They also ensure that medication adjustments are appropriate. Women should also be aware of potential side effects. They should report any concerns to their healthcare provider promptly. This proactive approach ensures optimal medication management. This ensures the best possible outcomes.
Managing Symptoms: Addressing Common Challenges
The menstrual cycle can bring various symptoms. These symptoms can impact diabetes management. Common symptoms include bloating, mood swings, and fatigue. These symptoms can affect blood sugar levels. They can also make diabetes management more challenging. Women should implement strategies to manage these symptoms. These strategies promote overall well-being. Women should prioritize adequate sleep. They should aim for seven to eight hours of sleep per night. This helps regulate blood sugar levels. It also helps improve mood and energy levels.
Stress management techniques are also beneficial. Women should practice relaxation techniques like deep breathing or meditation. These techniques can reduce stress. They can also improve mood. Over-the-counter medications can help manage specific symptoms. Women should consult with their healthcare provider. They should discuss the use of these medications. They should also discuss potential interactions with diabetes medications. Managing these symptoms can help women feel better. It can also improve diabetes management.
Collaboration and Support: Building a Strong Team
Managing diabetes during the menstrual cycle is easier with support. Women should build a strong healthcare team. This team should include a primary care physician, an endocrinologist, and a certified diabetes educator. These professionals provide expert guidance. They also offer personalized support. Women should openly communicate with their healthcare team. They should discuss their experiences and challenges. This communication allows for tailored strategies. It also ensures optimal outcomes. Support groups and online communities can also provide valuable resources. These resources include emotional support. They also provide practical advice. [See also: The Benefits of Diabetes Support Groups]
Family and friends can also play a vital role. Women should educate their loved ones. They should teach them about their diabetes management plan. This education helps foster understanding and support. This support can make a significant difference. It can improve overall well-being. Building a strong support system is essential. It helps navigate the challenges of diabetes. It also ensures a better quality of life.
When to Seek Professional Help
While most women can manage their diabetes during the menstrual cycle, some situations require professional intervention. Women should seek immediate medical attention if they experience frequent or severe hypoglycemia or hyperglycemia. They should also seek help if they have any unexplained changes in blood sugar control. Other concerning symptoms include infections or other health issues. These symptoms may require adjustments to the diabetes management plan. They may also require medical attention. Seeking professional help is crucial. This ensures the best possible health outcomes. It also prevents complications.
Long-Term Health: Prioritizing Overall Well-being
Successfully managing diabetes during the menstrual cycle is about more than just blood sugar control. It’s about prioritizing overall well-being. Women should focus on healthy lifestyle choices. They should maintain a balanced diet. They should exercise regularly. They should also prioritize sleep and stress management. These habits promote long-term health. They also reduce the risk of diabetes-related complications. They should also attend regular check-ups. These check-ups are important for monitoring overall health. They also help identify and address any potential issues. [See also: Long-Term Complications of Diabetes]
By adopting a holistic approach, women can effectively manage diabetes. They can do this during the menstrual cycle. They can also improve their quality of life. This improved quality of life includes physical health. It also includes emotional and mental well-being. This comprehensive strategy empowers women. It empowers them to live fulfilling lives. It allows them to be healthy and thriving.
Conclusion: Taking Control of Your Health
Managing diabetes during the menstrual cycle requires knowledge. It requires proactive strategies. It also requires a commitment to self-care. By understanding the impact of hormones. By tracking blood sugar levels and making appropriate adjustments. Women can effectively navigate the challenges. They can also maintain stable blood sugar levels. They can improve their overall health. Remember, consistency is key. Work closely with your healthcare team. Embrace a healthy lifestyle. Take control of your health. You can live a fulfilling life. You can live well with diabetes. The key is understanding how to control diabetes during the menstrual cycle.