How to Reduce Inflammation and Help Diabetes: A Comprehensive Guide
The intricate dance between inflammation and diabetes is a topic of significant interest to both medical professionals and individuals seeking to improve their health. Chronic inflammation is increasingly recognized as a key player in the development and progression of type 2 diabetes. This article delves into the connection between inflammation and diabetes, exploring the mechanisms involved and, most importantly, providing actionable strategies on how to reduce inflammation and help manage diabetes effectively. We will investigate practical lifestyle changes and dietary modifications that can empower individuals to take control of their health.
Understanding the Link: Inflammation and Diabetes
Inflammation, the body’s natural response to injury or infection, becomes problematic when it persists at a chronic, low level. This persistent inflammation can disrupt the body’s metabolic processes, significantly increasing the risk of developing type 2 diabetes. The connection is complex, but key factors are at play.
One of the primary mechanisms involves insulin resistance. Chronic inflammation can interfere with insulin signaling, making cells less responsive to insulin. This resistance forces the pancreas to produce more insulin, eventually leading to its exhaustion and a rise in blood sugar levels. Moreover, inflammation can damage the insulin-producing beta cells in the pancreas, further impairing insulin production. This is a direct link on how to reduce inflammation and help diabetes.
Several inflammatory markers are associated with diabetes. These include C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α). Elevated levels of these markers are often found in individuals with diabetes and those at risk of developing the condition. These inflammatory markers are crucial to understanding how to reduce inflammation and help diabetes. The inflammatory response contributes to the development of insulin resistance. It also contributes to the damage of pancreatic beta cells.
Dietary Strategies: Fueling Your Body for Health
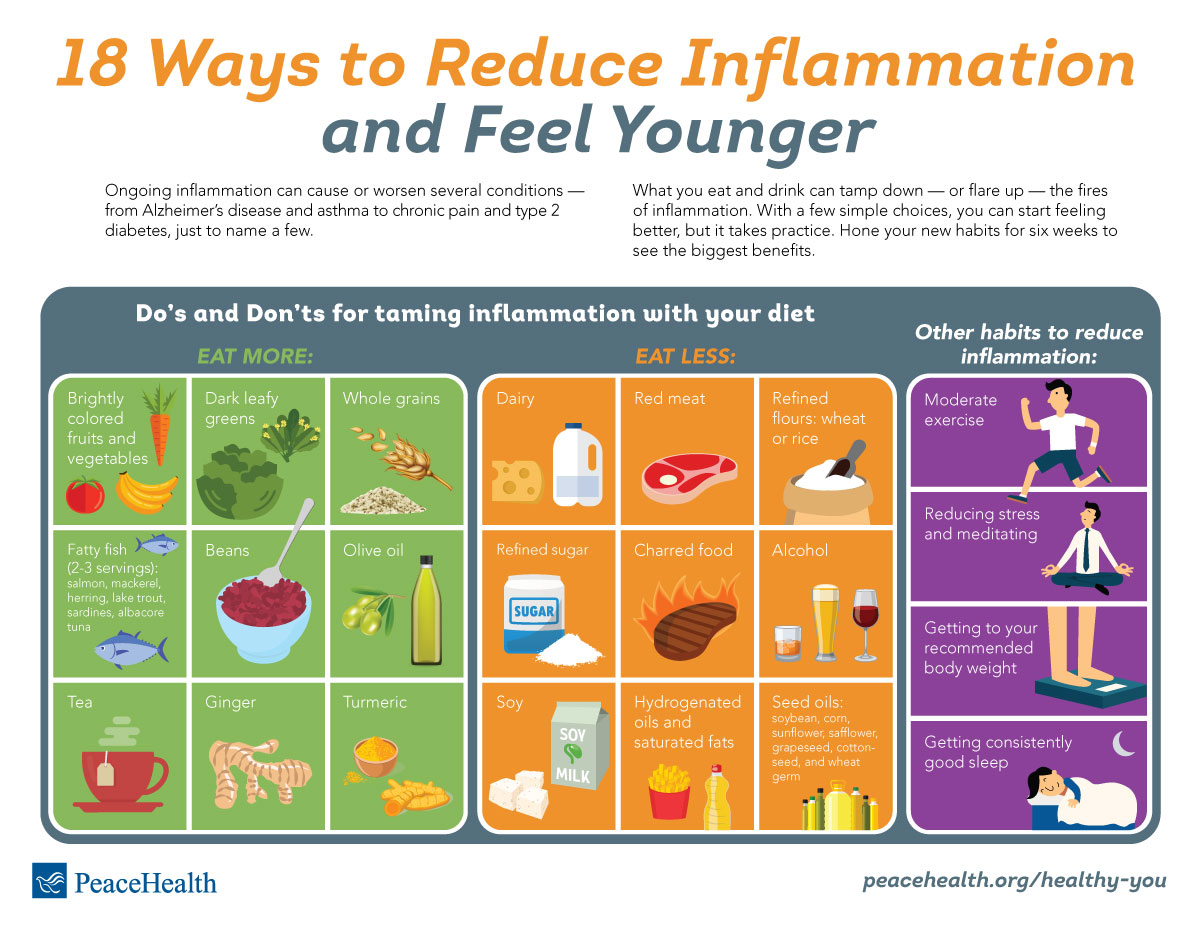
Diet plays a pivotal role in managing inflammation and diabetes. Certain foods can exacerbate inflammation, while others possess potent anti-inflammatory properties. Making informed dietary choices is a cornerstone of any plan on how to reduce inflammation and help diabetes.
Embracing an Anti-Inflammatory Diet
An anti-inflammatory diet emphasizes whole, unprocessed foods. It is rich in fruits, vegetables, lean proteins, and healthy fats. Focus on foods that are naturally low in sugar and high in fiber. This approach helps regulate blood sugar levels and reduce inflammation simultaneously.
Key components include:
- Fruits and Vegetables: Load up on colorful produce. Berries, leafy greens, and cruciferous vegetables (broccoli, cauliflower) are packed with antioxidants and anti-inflammatory compounds.
- Healthy Fats: Incorporate sources of omega-3 fatty acids, like fatty fish (salmon, mackerel) and flaxseeds. These fats help combat inflammation.
- Lean Protein: Choose lean protein sources such as fish, poultry, beans, and lentils. These provide essential nutrients without contributing to inflammation.
- Whole Grains: Opt for whole grains like oats, quinoa, and brown rice over refined grains. These provide fiber and help regulate blood sugar levels.
Foods to Limit or Avoid
Certain foods are known to promote inflammation. Limiting or avoiding these is crucial for managing both inflammation and diabetes. This is an essential step on how to reduce inflammation and help diabetes.
- Processed Foods: These are often high in sugar, unhealthy fats, and additives that trigger inflammation.
- Sugary Drinks: Sodas, juices, and other sweetened beverages contribute to high blood sugar levels and inflammation.
- Refined Carbohydrates: White bread, pasta, and other refined grains can cause rapid spikes in blood sugar.
- Excessive Red Meat: Some studies suggest a link between high red meat consumption and increased inflammation.
- Trans Fats: Found in many processed foods, trans fats are strongly associated with inflammation.
Lifestyle Modifications: Beyond the Plate
Diet is only one piece of the puzzle. Lifestyle modifications play a crucial role in controlling inflammation and managing diabetes. Regular physical activity, stress management, and adequate sleep are all essential components.
Regular Physical Activity
Exercise has potent anti-inflammatory effects. It improves insulin sensitivity, helps regulate blood sugar levels, and promotes overall health. Aim for at least 150 minutes of moderate-intensity exercise per week. This is a key factor on how to reduce inflammation and help diabetes.
Consider a combination of aerobic exercise (walking, running, swimming) and strength training. Find activities that you enjoy to make exercise a sustainable part of your routine.
Stress Management Techniques
Chronic stress can exacerbate inflammation and worsen diabetes symptoms. Implementing stress management techniques is vital. This is also a key aspect of how to reduce inflammation and help diabetes.
Effective techniques include:
- Mindfulness Meditation: Practicing mindfulness can reduce stress and promote a sense of calm.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation to reduce stress and improve overall well-being.
- Deep Breathing Exercises: These can help calm the nervous system and reduce stress.
- Spending Time in Nature: Exposure to nature has been shown to reduce stress levels.
Prioritizing Sleep
Adequate sleep is crucial for overall health and can influence inflammation and blood sugar control. Aim for 7-9 hours of quality sleep per night. Sleep deprivation can increase inflammation and worsen insulin resistance.
Establish a regular sleep schedule. Create a relaxing bedtime routine. Ensure your bedroom is dark, quiet, and cool. If you have trouble sleeping, consult with a healthcare professional.
Supplements and Medications: When to Seek Professional Guidance
While lifestyle changes are foundational, some individuals may benefit from supplements or medications to manage inflammation and diabetes. It is essential to consult with a healthcare professional before starting any new supplements or medications.
Potential Supplements
Several supplements have shown promise in reducing inflammation and improving blood sugar control. However, their effectiveness can vary. Also, they may interact with medications.
- Omega-3 Fatty Acids: These can reduce inflammation and improve insulin sensitivity.
- Curcumin: The active compound in turmeric has potent anti-inflammatory properties.
- Alpha-Lipoic Acid (ALA): This antioxidant can improve insulin sensitivity.
- Berberine: This supplement may help lower blood sugar levels.
Diabetes Medications
For individuals with diabetes, medications play a crucial role in managing blood sugar levels. These medications can also have indirect effects on inflammation.
Common diabetes medications include:
- Metformin: This medication helps improve insulin sensitivity.
- Sulfonylureas: These stimulate the pancreas to produce more insulin.
- GLP-1 Receptor Agonists: These medications help lower blood sugar levels and may have anti-inflammatory effects.
- SGLT2 Inhibitors: These medications help remove excess glucose from the body through urine.
Always discuss medication options with your healthcare provider. They can determine the most appropriate treatment plan for your specific needs.
Monitoring and Managing Your Health
Regular monitoring is essential for managing both inflammation and diabetes. This includes monitoring blood sugar levels, tracking inflammatory markers, and working closely with your healthcare team. This is a core practice on how to reduce inflammation and help diabetes.
Blood Sugar Monitoring
Regularly monitor your blood sugar levels. This helps you understand how your body responds to food, exercise, and medications. Aim for target blood sugar levels as recommended by your healthcare provider. This is an essential practice for how to reduce inflammation and help diabetes.
Tracking Inflammatory Markers
Discuss with your doctor the possibility of testing inflammatory markers. This can provide insights into your body’s inflammatory state. Markers like CRP and IL-6 can be monitored over time to assess the effectiveness of your interventions.
Working with a Healthcare Team
Build a strong relationship with your healthcare team. This includes your doctor, registered dietitian, and certified diabetes educator. They can provide personalized guidance and support to help you manage your health. Following their advice is the best method on how to reduce inflammation and help diabetes.
The Path Forward: A Proactive Approach
Taking a proactive approach to your health is critical for managing inflammation and diabetes. By understanding the link between these two conditions and implementing the strategies outlined in this guide, you can significantly improve your health outcomes. Remember that consistency is key. Making sustainable lifestyle changes is more effective than quick fixes. This is a summary on how to reduce inflammation and help diabetes.
Prioritize a balanced diet, regular physical activity, effective stress management, and adequate sleep. Consult with your healthcare provider to develop a personalized plan. They can tailor a plan to your specific needs. By taking these steps, you can reduce inflammation and help manage diabetes, ultimately improving your quality of life. This is the best way on how to reduce inflammation and help diabetes.
[See also: Related Article Titles]