How to Eat for Diabetes While Intermittent Fasting: A Comprehensive Guide
Intermittent fasting (IF) has gained significant popularity as a dietary approach for weight management and overall health improvement. For individuals with diabetes, the combination of IF and managing blood sugar levels presents a unique set of considerations. This article provides a comprehensive guide on how to eat for diabetes while intermittent fasting, covering the key aspects of this approach, from understanding the benefits and risks to practical strategies and meal planning.
Understanding the Basics: Diabetes and Intermittent Fasting
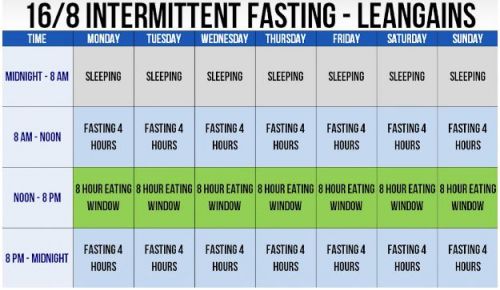
Diabetes, a metabolic disorder, is characterized by elevated blood sugar levels (hyperglycemia). There are two main types: Type 1, where the body doesn’t produce insulin, and Type 2, where the body doesn’t use insulin properly. Intermittent fasting involves cycling between periods of eating and voluntary fasting on a regular schedule. This can range from daily time-restricted eating (e.g., 16/8 method) to alternate-day fasting. The primary goal of how to eat for diabetes while intermittent fasting is to manage blood sugar levels effectively while potentially promoting weight loss and other health benefits.
Benefits and Risks: Weighing the Options
Potential Benefits
- Improved Insulin Sensitivity: IF can enhance the body’s response to insulin, which helps regulate blood sugar levels.
- Weight Management: IF may lead to weight loss, which can improve insulin resistance and overall health.
- Reduced Inflammation: Some studies suggest IF can reduce chronic inflammation, a factor linked to diabetes complications.
- Cellular Repair: During fasting periods, the body initiates cellular repair processes like autophagy.
Potential Risks
- Hypoglycemia (Low Blood Sugar): Without careful planning, IF can increase the risk of dangerously low blood sugar levels, especially for those on insulin or certain diabetes medications.
- Medication Adjustments: People with diabetes may need adjustments to their medication dosages to avoid hypoglycemia during fasting periods. This requires close consultation with a healthcare provider.
- Nutritional Deficiencies: Improper meal planning during eating windows can lead to nutrient deficiencies.
- Dehydration: Fasting can increase the risk of dehydration.
Consulting Your Healthcare Provider: A Crucial First Step
Before embarking on intermittent fasting, it is essential to consult with a doctor or a certified diabetes educator. They can assess your individual health status, medication regimen, and overall suitability for IF. Your healthcare team will help you determine the safest and most effective approach to how to eat for diabetes while intermittent fasting. This consultation should cover medication adjustments, blood sugar monitoring strategies, and personalized meal planning guidelines.
Practical Strategies: Eating for Diabetes During Intermittent Fasting
Choosing an Intermittent Fasting Method
Several IF methods can be considered, but the best one depends on individual preferences and lifestyle. The 16/8 method (16 hours of fasting and an 8-hour eating window) is a common choice. Other options include the 5:2 diet (eating normally for five days and restricting calories for two non-consecutive days), or alternate-day fasting. When deciding how to eat for diabetes while intermittent fasting, it is essential to start slowly. Begin with shorter fasting periods and gradually increase the duration as your body adapts. This approach minimizes the risk of adverse effects and allows for better blood sugar control.
Meal Planning: What to Eat
Meal planning is crucial when learning how to eat for diabetes while intermittent fasting. The focus should be on nutrient-dense foods that help manage blood sugar levels. This includes:
- Non-Starchy Vegetables: Load up on leafy greens, broccoli, cauliflower, and other low-carb vegetables.
- Lean Protein: Include sources like fish, poultry, beans, and tofu to help you feel full and maintain muscle mass.
- Healthy Fats: Incorporate sources like avocados, nuts, seeds, and olive oil.
- Complex Carbohydrates: Choose whole grains, such as quinoa, brown rice, and oats, in moderation.
- Limit Processed Foods: Avoid sugary drinks, processed snacks, and refined carbohydrates.
- Monitor Carbohydrate Intake: Count carbohydrates at each meal.
Sample Meal Plan
Here is a sample meal plan to guide you on how to eat for diabetes while intermittent fasting (16/8 method):
- Eating Window (12 PM – 8 PM):
- Lunch (12 PM): Large salad with grilled chicken, mixed greens, and a light vinaigrette.
- Snack (3 PM): A handful of almonds and a small apple.
- Dinner (6 PM): Baked salmon with roasted vegetables (broccoli, carrots) and a side of quinoa.
- Fasting Window (8 PM – 12 PM): Drink water, unsweetened tea, or black coffee.
Blood Sugar Monitoring
Regular blood sugar monitoring is vital when learning how to eat for diabetes while intermittent fasting. Check your blood sugar levels before, during, and after your eating and fasting windows. This helps you understand how your body responds to IF and allows you to make necessary adjustments to your diet, medication, or fasting schedule. Keep a detailed log of your blood sugar readings and any symptoms of hypoglycemia or hyperglycemia.
Hydration and Electrolytes
Staying hydrated is crucial when learning how to eat for diabetes while intermittent fasting. Drink plenty of water throughout the day, especially during fasting periods. Consider adding a pinch of salt to your water or consuming electrolyte-rich beverages to maintain electrolyte balance. This is particularly important if you experience symptoms like dizziness or headaches.
Medication Management: A Critical Consideration
If you take medications for diabetes, it is essential to work closely with your healthcare provider to adjust your dosages as needed. This is a key aspect of how to eat for diabetes while intermittent fasting. Insulin and certain oral medications can increase the risk of hypoglycemia during fasting. Your doctor may advise you to reduce your medication doses or change the timing of your medication administration to match your eating schedule. Never adjust your medication without professional medical advice.
Managing Potential Side Effects
Intermittent fasting can cause side effects, such as headaches, fatigue, and dizziness. These effects are often temporary and can be minimized with proper planning. If you experience any concerning side effects, such as severe hypoglycemia or persistent symptoms, consult your doctor immediately. Here are tips for managing common side effects when learning how to eat for diabetes while intermittent fasting:
- Headaches: Stay hydrated and ensure you’re getting enough electrolytes.
- Fatigue: Make sure you are eating enough calories during your eating window.
- Dizziness: Stand up slowly and stay hydrated.
Long-Term Sustainability and Lifestyle Adjustments
Sustainability is key to the long-term success of intermittent fasting. Choose an IF method that fits your lifestyle and preferences. Make sure that you are able to stick to your fasting and eating schedule over time. Incorporate regular physical activity into your routine. Exercise can improve insulin sensitivity and contribute to better blood sugar control. Focus on a balanced diet. This will help you manage your blood sugar levels and support your overall health.
Conclusion: Mastering the Art of Eating for Diabetes While Intermittent Fasting
Successfully implementing intermittent fasting for diabetes management requires a thoughtful and informed approach. By understanding the benefits and risks, working closely with your healthcare provider, and following a well-planned diet and lifestyle, you can learn how to eat for diabetes while intermittent fasting effectively and safely. Remember, consistency, monitoring, and professional guidance are key to achieving your health goals. [See also: Related Article Titles]
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Consult with a healthcare professional before starting any new dietary regimen or making changes to your medication.